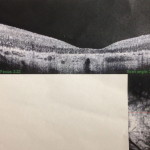
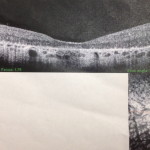
If you’re wondering what these two ultrasound-looking photos are, they are actually photos of my retinas taken at my most recent appointment. Like I said in Part 1, I learned a lot at this appointment, and the photos were just part of this wealth of information.
While I knew that I had a form of RP known as Lebers, I hadn’t realized that a 1995 blood test revealed the specific RP gene that Jenelle and I have; it is called the CRB1 Gene. This gene, unfortunately, is not the specific gene in clinical trials for gene therapy right now (the treatment that Dr. Fishman feels is the most promising within the near future).
Another gene, the RPE65 gene, is currently in human trials, and from what I gathered from Dr. Fishman, this is mostly due to the fact that it is one of the more common RP genes and that patients with RPE65 tend to have their central nuclear still intact, a necessary requirement for gene therapy
This is a new term I learned today, and they actually took pictures of my retinas to see if my central nuclears were still viable, meaning that the cells are alive and could therefore be receptive to gene therapy. This is, of course, all hypothetical considering the CRB1 gene is not currently in clinical trials. I naively asked whether it would be the next gene in trials, not realizing that there are many other RP genes that have also been identified that would be in the running. He said that research studies are more likely to take place with the genes that affect the most amount of people first. When asked how common the CRB1 gene is, he said it’s right in the middle. So there may be some waiting. He said that the results for the RPE65 gene are promising so far, however, and that once the initial FDA-approval process is over with, the following trials will be able to move at a much faster pace than the first one. Of course, even if the CRB1 gene begins human trials in the near future, Dr. Fishman pointed out that there are still many risks to weigh in whether Jenelle and I would want to volunteer to be among some of the first groups for treatment, especially considering they have to detach your retina during surgery, which could potentially decrease vision even further.
Dr. Fishman himself is involved more directly in some pharmacological studies that do similar work as gene therapy but are taken as medication rather than surgery. Some patients have had improved fields from this drug study, though the patient he was specifically testing did not have improved fields (but improved his acuity by 17 letters, which is substantial).
These are pictures of my retinas. The dark area in the periphery is scarring, or as Dr. Fishman put it, “charcoal ashes from the fire that is the disease”. The small white area in the center shows my central nuclear, which is still intact, though it is a very thin layer. The center of everyone’s retina is thin, but is extremely thin in patients with RP.
As far as other results from this visit, one major disappointment from Dr. Fishman moving offices is that a lot of records did not make it over yet, including my previous visual fields tests. I had been anxious to compare the results of today’s test to previous tests, but such is life Hopefully they will eventually find all of their files.
I did feel like my fields were pretty narrow during the test, but I think I am always surprised by how much I really can’t see when I take the fields test. Marty, my favorite technician who was doing my test, was particularly astonished that in my left eye– the one that can’t even see the giant E on the chart at 20/400, could still see a tiny pen-light in the center of the field test “All-be-darn” was his exact quote. Again, since they don’t have my previous records at the moment, I have no idea whether this is something I could see during my previous tests 3 years ago. While I did a fields test at my local eye doctor in Naperville this past fall, the test was not nearly as thorough, and the technician got really confused while doing the test because she had never done a test on someone with such low vision before, so I can’t use that one to compare to either.
Marty also said that he finds it fascinating how I am able to even walk from the waiting room to the exam room without any problem. He remarked on how the human brain compensates for the missing pieces of vision and fills vision in to make things look like a whole picture when there should really be no way to see the whole picture at all. He said with the vision I have, even walking around should be nearly impossible, but because my brain has filled in these pieces, I’m able to (even if it’s not always very well!) While I have had many of these same thoughts before, I was never sure if they had any actual scientific basis to them before hearing a professional say them.
As I said in Part 1, Dr. Fishman’s care for his patients was particularly evident to me during this visit I’m not sure whether it’s the new office environment or whether maybe I’m just better at asking specific questions now as an adult, but I feel like he took such care explaining extremely complicated scientific information in simple terms that I could understand.
I definitely plan on recording my next visit so that I can actually listen to it once I get home since there is way too much information to even begin to remember, much less reiterate to my family and friends later. Until then, I hope my modest attempt to convey pieces of info from the visit is helpful. Thanks for reading!